Milk Donation 2022 of Rainbow Mother’s Milk Bank Banjara Hills
Total Donation
Total Dispensed
Milk Donation









It can help save a life. Your donation of milk to the milk bank can enable babies to access the benefits of breast milk who, for some reason, may otherwise be deprived of it.
- Premature babies and sick babies, whose mother is unable to provide them their own milk.
- Babies whose mothers are suffering from postpartum illness.
- Babies whose mother are having lactation failure or the milk output is insufficient.
- Babies who have been adopted and mothers are not lactating.
- Babies who’ve lost their mother.
Any healthy lactating mother who
- Is in good health, and not on any regular medication or supplements (except for prenatal vitamins, nasal sprays, human insulin, thyroid replacement hormones, eye drops, asthma inhalers, topical treatments, progestin only or low dose estrogen birth control products)
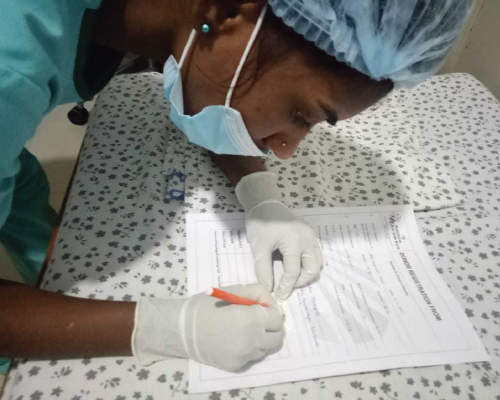
- Is ok to undergo screening (blood testing) for infections
- Has excess milk to spare after feeding her baby
You may be able to donate your extra breast milk if you are:
- In good general health
- Willing to complete a screening questionnaire and have a blood test
- Not currently taking most medications (except some supplements)
- Free from smoking, illegal drug use and regular alcohol use
Bereaved mothers who wish to donate their breast milk to help another baby are also welcomed.
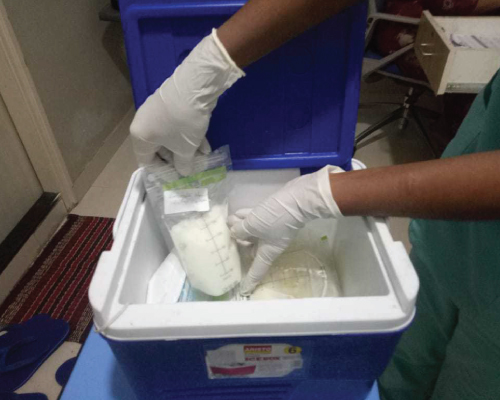
Breast milk that has been donated to a milk bank and pasteurized in a heat treatment process that
eliminates harmful bacteria/viruses.
The pasteurization process is similar to that used to ensure the safety of cow’s milk.
Pasteurized donor milk goes through a rigorous testing process to ensure its safety.
Most of the unique nutrients and components (such as immune factors) found only in human breast milk are retained after pasteurization. There are slightly lower levels of some nutrients however all babies in the NICU have their growth monitored.
The Milk Bank follows guidelines set by the Human Milk Banking Association of North America (HMBANA) and public health regulations governing the handling, processing and storage of food.
Every effort will be made to feed the baby with mother’s own milk prior to using donor milk. When there is not enough of mother’s own milk, babies may receive donor milk for several weeks during their hospitalization. At the end of this time, if there is not enough of mother’s own milk, babies will be transitioned to an appropriate formula.
The baby’s growth will be monitored as some babies grow slower, and may require nutritional
supplementation.
In decades of human milk banking worldwide, there have been no published reports of infectious
diseases being caused by properly pasteurized human donor milk. The risk of infection, however
slight, cannot be reduced to zero just as is the case with the use of blood products.
No. Milk donations are strictly on a voluntary basis.
No. Donor milk is provided free of charge to hospitalized babies by prescription.
Protection from infection: Donor breast milk contains many of the protective factors (such
as immunoglobulins) which help protect babies from infection.
Protection from necrotizing enter colitis: Donor breast milk may also have protective
role against the serious gut condition necrotizing enterocolitis which mainly affects premature
babies.
Easier to digest: A premature baby’s gut is very immature and is able to digest and
absorb breastmilk more easily than formula milk. Premature babies are fed small amounts of
breastmilk to help their gut mature and the volumes fed are increased gradually. This is also true
for babies who have had gut surgery.

