Categories
Neurosonogram and Common Doubts
Feb 13, 2025
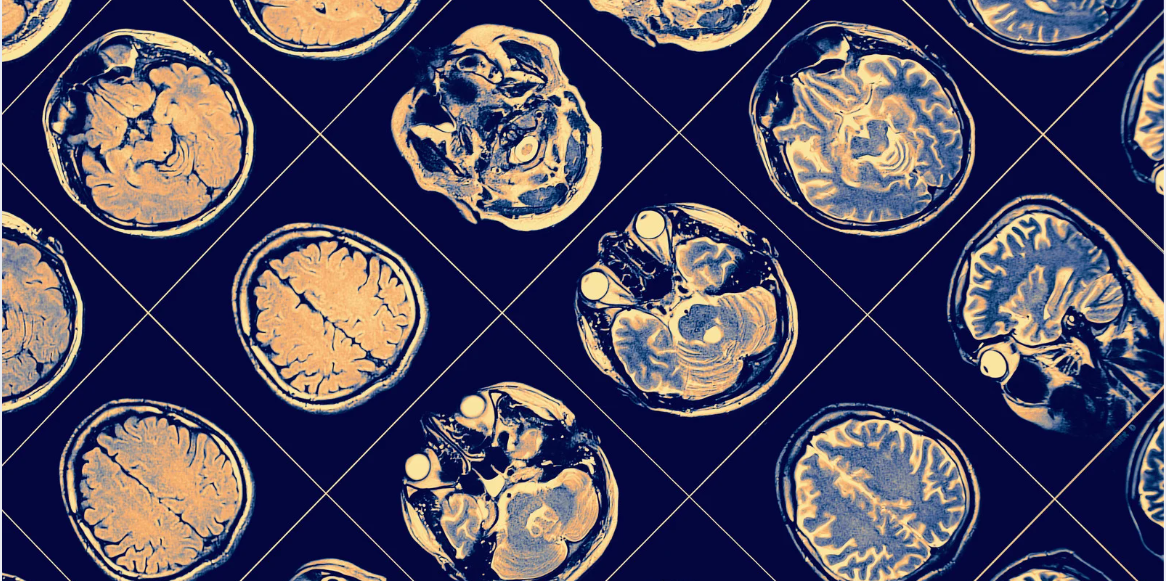
A neurosonogram,
also known as a cranial ultrasound,
is an imaging test that uses sound waves
to visualize a newborn baby’s brain. Since the bones of the skull are not fully
formed at birth, the soft spot
(fontanelle) on the top of the baby’s head serves as a natural window for
ultrasound to assess the brain. Additional windows, such as the posterior and mastoid fontanelles, may
also be used for better evaluation.
Neurosonography is most reliable in babies under six months old, as the fontanelle gradually closes over time. This test is portable and can be performed bedside in neonatal intensive care units (NICUs) or in the radiology department. However, it has limitations—some deeper or peripheral areas of the brain may not be fully visualized.
Is it Safe?
Yes, cranial ultrasound is very safe. Unlike CT scans or X-rays, it does not use ionizing radiation, making it a preferred radiation-free imaging modality for newborns. Radiologists take care to minimize scan duration while ensuring a thorough evaluation.
When is it Done?
A neurosonogram is a valuable tool for detecting various intracranial conditions,
including:
●
Congenital anomalies
● Brain infections
With advancements in neonatal care, preterm babies can now be managed effectively in NICUs until they are stable enough for discharge. However, due to their increased risk of brain-related complications, routine neurosonogram are often performed, especially in preterm infants.
Routine Neurosonogram
Schedule for Preterm Infants:
Depending on hospital protocols,
premature babies may undergo serial
neurosonograms at specific intervals, such as:
●
Day 0 (at birth)
●
Day 28
In some cases, follow-up neurosonograms may be required even after discharge to
monitor for late-developing changes in the brain.
Common Doubts Regarding
Neurosonogram Reports
1. What does
"Periventricular Flare" mean?
"Periventricular flare," also called periventricular echogenicity (PVE), appears as a brighter-than-usual area near the
fluid-filled spaces (ventricles) of the brain. This region is particularly vulnerable to ischemic (low oxygen) injury
due to its delicate blood supply in preterm infants.
However, PVE can have multiple causes:
●
It may be a normal variant
●
In a few cases, it may progress to
periventricular leukomalacia (PVL), a form of brain injury - which is best
understood clinically.
Since ultrasound findings should never be interpreted in isolation, a
discussion with your pediatrician or
neonatologist is essential to understand the clinical significance.
2. What is a
"Germinal Matrix Hemorrhage" (GMH)?
A germinal
matrix hemorrhage (GMH) is a bleed
in a specific region of the brain called the caudothalamic groove, which contains fragile blood vessels. This is
one of the most common sites of bleeding
in preterm infants due to their immature vascular system.
Grading
of GMH:
●
Grade 1 GMH means the bleeding is limited to the caudothalamic groove.
●
Grade 1 hemorrhages are common and often resolve on their own.
While mild hemorrhages are generally not worrisome, follow-up ultrasounds
are recommended to monitor their progression. Your pediatrician will guide you on the next steps based on your
baby’s condition.
What Should You Do?
●
A clear discussion with your neonatologist or pediatrician is crucial
in interpreting neurosonogram findings.
●
Follow-up scans may be needed for better
assessment over time.
Limitations of Neurosonogram
●
Some areas of the brain may not be
well visualized due to the limited
ultrasound penetration through bone.
●
Interpretation should always be done in conjunction with clinical
findings.
Final Thoughts
A neurosonogram
is a safe, effective, and widely used tool for evaluating newborn brain
health. However, understanding the context
of the findings is key. Your healthcare
team is the best resource for discussing the results and any necessary next
steps.
References
- Bellar, T., Peylan, T., Ben-Sira. Quantitative analysis of cranial
ultrasonographic periventricular echogenicity in relation to early
neuromotor development in preterm infants.